INTRODUCTION
4 TRENDS IN MOB DESIGN AND DEVELOPMENT
Introduction
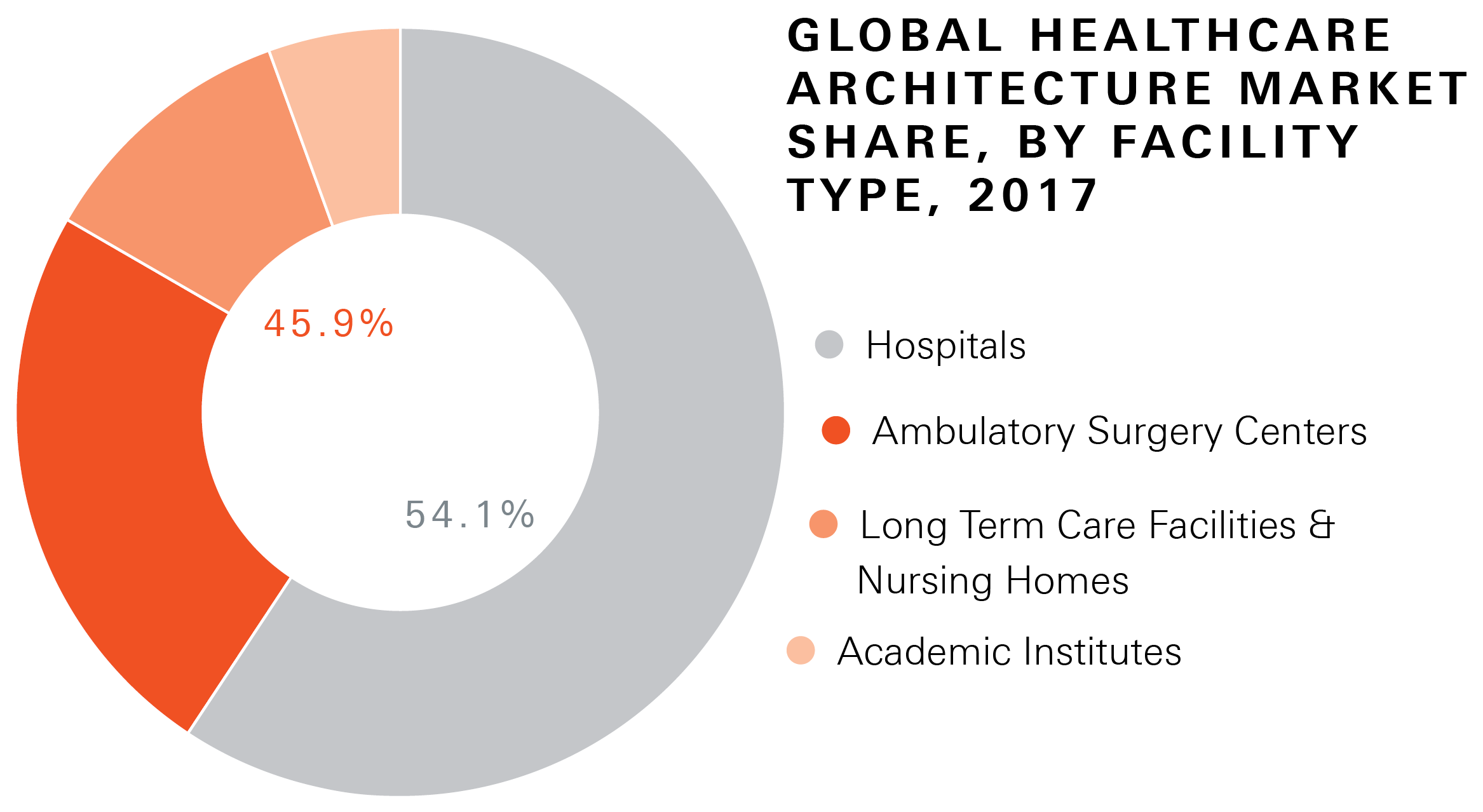
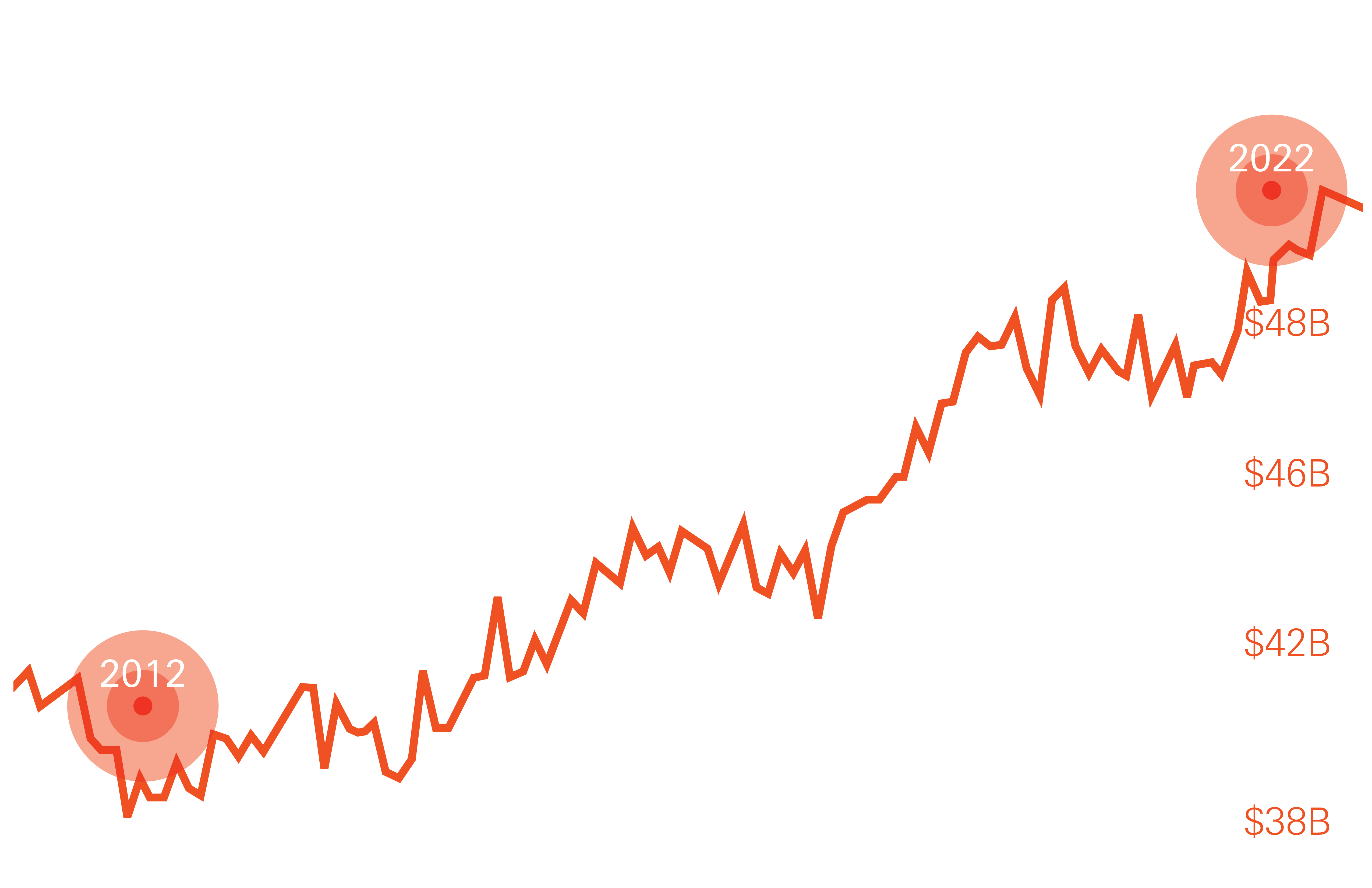
Healthcare construction in 2022 was a $53.98B industry in the U.S., growing at a 4% CAGR for over 20 years, according to the Federal Reserve.
A large driver of that growth has been the acceleration of a subcategory of healthcare called “medical office buildings (MOB).” These facilities are constructed for non-hospital medical uses that can range from fertility clinics to ambulatory outpatient surgery centers.
In 2021 the amount of square footage occupied by such non-hospital healthcare uses reached equivalency with hospital usage facilities for the first time in history. (https://revistamed.com/amount-of-mob-space-now-equals-that-of-hospitals/).
The driver behind MOB development is very often cost-related, because MOBs are not regulated by all of the same stringent building code requirements as hospitals. In some cases, location is more of a driver – a hospital provider might want to serve a community from within, where it may not already have real estate, or where it might be infeasible to construct a full hospital facility for one reason or another.
From a design and construction perspective, form follows function – understanding both the program and the organizational mission should inform any conceptualization. “MOB is one of those fungible terms,” explains Jean Mah, Global Healthcare Practice leader at Perkins & Will. “Some are developer-built core and shell buildings with leased spaces for multiple tenants, some house a single tenant, some are ambulatory care or outpatient surgery centers, some are imaging centers – and many are a hybrid of all things. My best advice to designers is to make sure you understand the intent and usage before you start thinking about program and design.”
This white paper will discuss several trends that are emerging in the field of MOB development, as they relate to a variety of different program and provider types – and will highlight best practices in design and development as presented by Mah and other professionals who bring decades of expertise to the conversation.
Graph: Total Construction Spending
on Healthcare in the United States
(in Billions)
TREND 1
MULTIDISCIPLINARY MOBS
Multidisciplinary MOBS
Whether single tenant or multi-tenant, there has been a realization over the last two decades that care is more efficient both for patients and providers when multiple disciplines are housed in one location.
Stan Chiu, Director of Healthcare Design for Gensler, has been a part of the MOB emerging sector for over 20 years, and explains that while the U.S. for decades has built MOBs to suit a one-to-one doctor on patient delivery system, he is watching a different model progress into the mainstream that he first saw tested at the Mayo Clinic many years ago.
“There is a shift toward team-based care, which drives a shift in infrastructure to support collaboration immediately in the clinical environment while supporting patient privacy, etc… The idea behind this is that a team of people provides better care than individual practitioners,” he explains. When it comes to planning the built environment, the multidisciplinary approach drives a very different building layout and concept.
“In the traditional form, if you were organized around a smaller team, you were also organized around smaller practices and smaller footprint offices. Each had its own lobby, support staff, lab, and exam room – and then you scaled it up to maybe 15-20 individual doctor practices per building. The prevailing building design for that model would typically feature a center core with a central corridor. The elevator and restrooms at the core, the corridor and offices wrapping around,” continues Chiu.
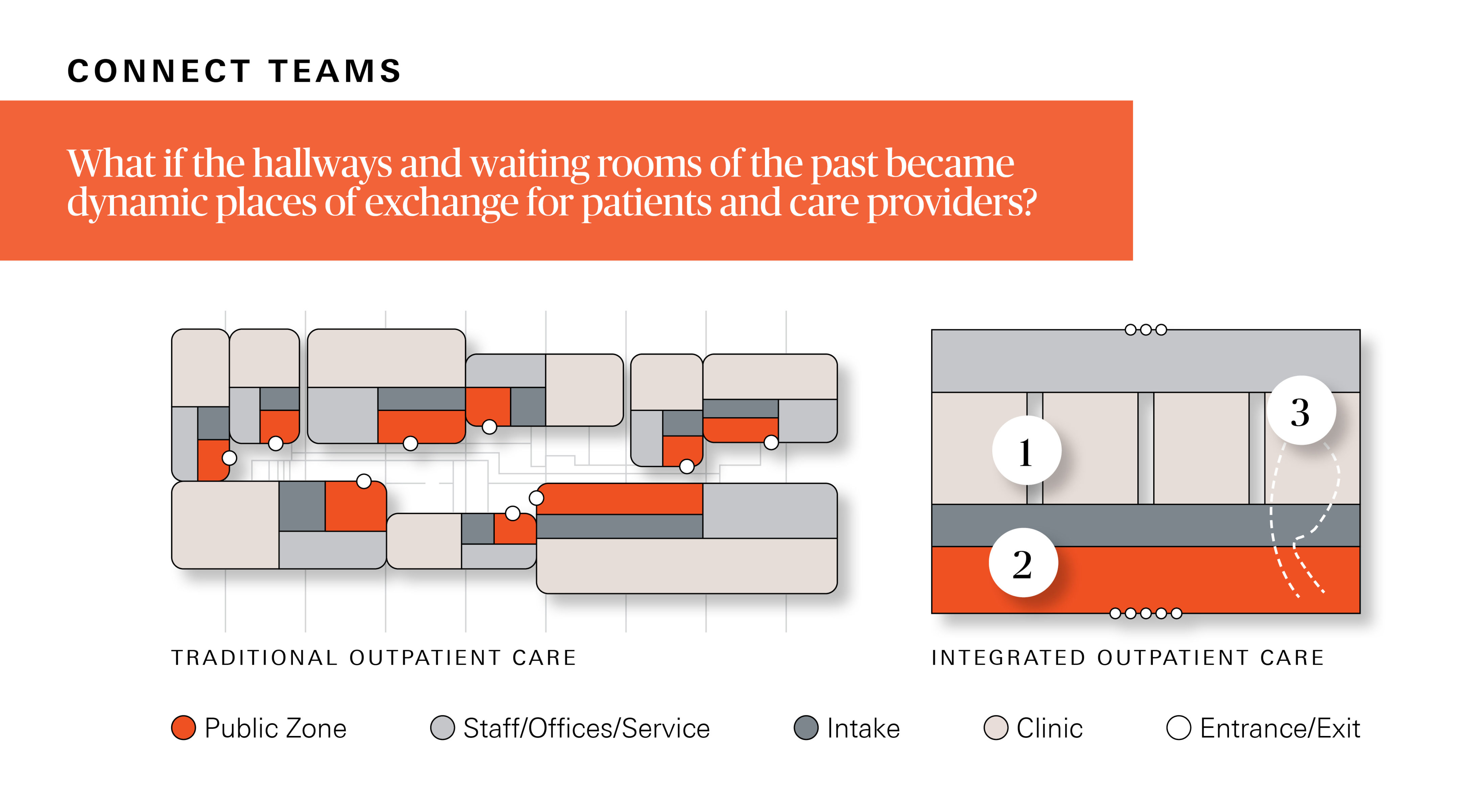
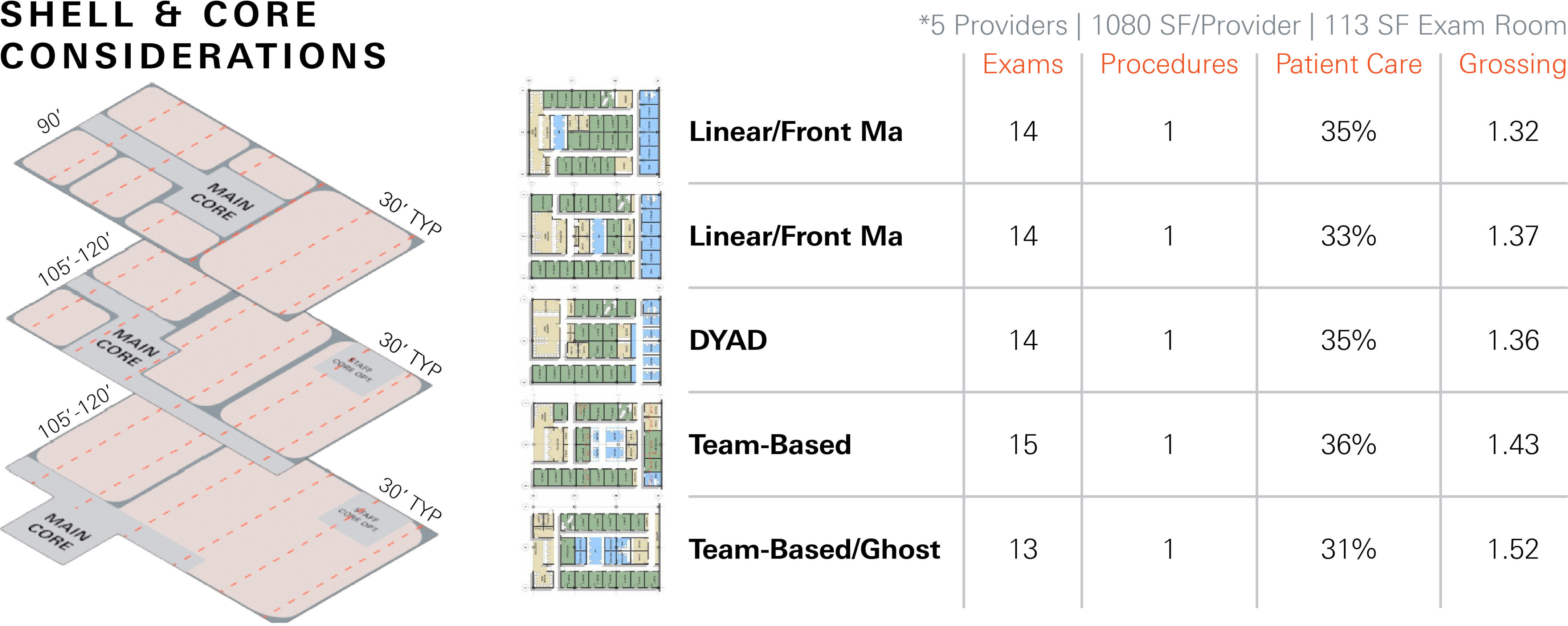
“The good thing about that,” Chiu says, “was that you could break the offices into small bits. The downside was that the circulation and public space was internal. At only about 90’ wide, you ended up with spaces only 40’ deep – not enough for a collaborative team environment of 4-6 people. The few practices that tried a more collaborative model found the buildings were very inefficient and just didn’t flow. The form of the building itself just didn’t support that model.”
Again, form follows function. In a multi-tenant building, ROI drives much of the design decision-making, and few buildings break out of traditional molds. “The multi-tenant MOB building is typically a double-loaded corridor of a certain depth that can house between 1,500-10,000sf per tenant,” says Jean Mah. “It’s a pretty definable dimension because every doctor’s office needs a window, a minimal corridor space, a minimal lobby – in order to achieve a certain leasing rate.”
By contrast, in multi-disciplinary team-based care environments, the vision is to keep collaborative space large and flexible – and for individual doctors to share access to diagnostic equipment, support staff, and labs.
“What we’re finding more and more is that the size of floor plates and the consolidation of health systems is that co-locating multidisciplinary practices – having blood draws, imaging, sometimes rehab, and even outpatient surgery centers makes it more efficient for the providers and more cost-effective for the patients,” says Jean Mah. “In our practice we are more focused on these owner-developed, build-to-suit or developer lease-back situations. In a multidisciplinary space, the floor plates are much larger, and we like the circulation to be peripheral so that the floor is flexible for different combinations of services over time. That’s perhaps the most significant design difference between this and a typical spec core and shell multi-tenant MOB.”
“But the structural design is quite nuanced,” she continues. “The more technology a program requires, the more we have to consider structural loading, vibration, having enough floor to floor height to accommodate ceiling mounted equipment, for things like MRIs, CTs and other imaging technology. The client’s cost model becomes different because capital cost is greater and HVAC systems are much more robust,” says Mah.
Chiu reflects on the emergence of a trend that started with his very first MOB project for the Mayo Clinic over 20 years ago. “At that time, the Mayo Clinic came along and we developed a building with them where the clinical part of the building was 100’ deep with nothing in it. It was a completely flexible space, similar to a retail, not medical building – and it could be organized to support teams of providers working collaboratively next to the clinical environment,” says Chiu. “Now all of the forward-looking providers are following suit. This means programmatically they are pulling the core outside of the center of the building and onto the perimeter so that the provider space is large and flexible”
TREND 2
REAL ESTATE DEVELOPMENT VS TAKING THE CARE TO THE COMMUNITY
Trend 2
Real Estate Development
vs. Taking the Care to the Community
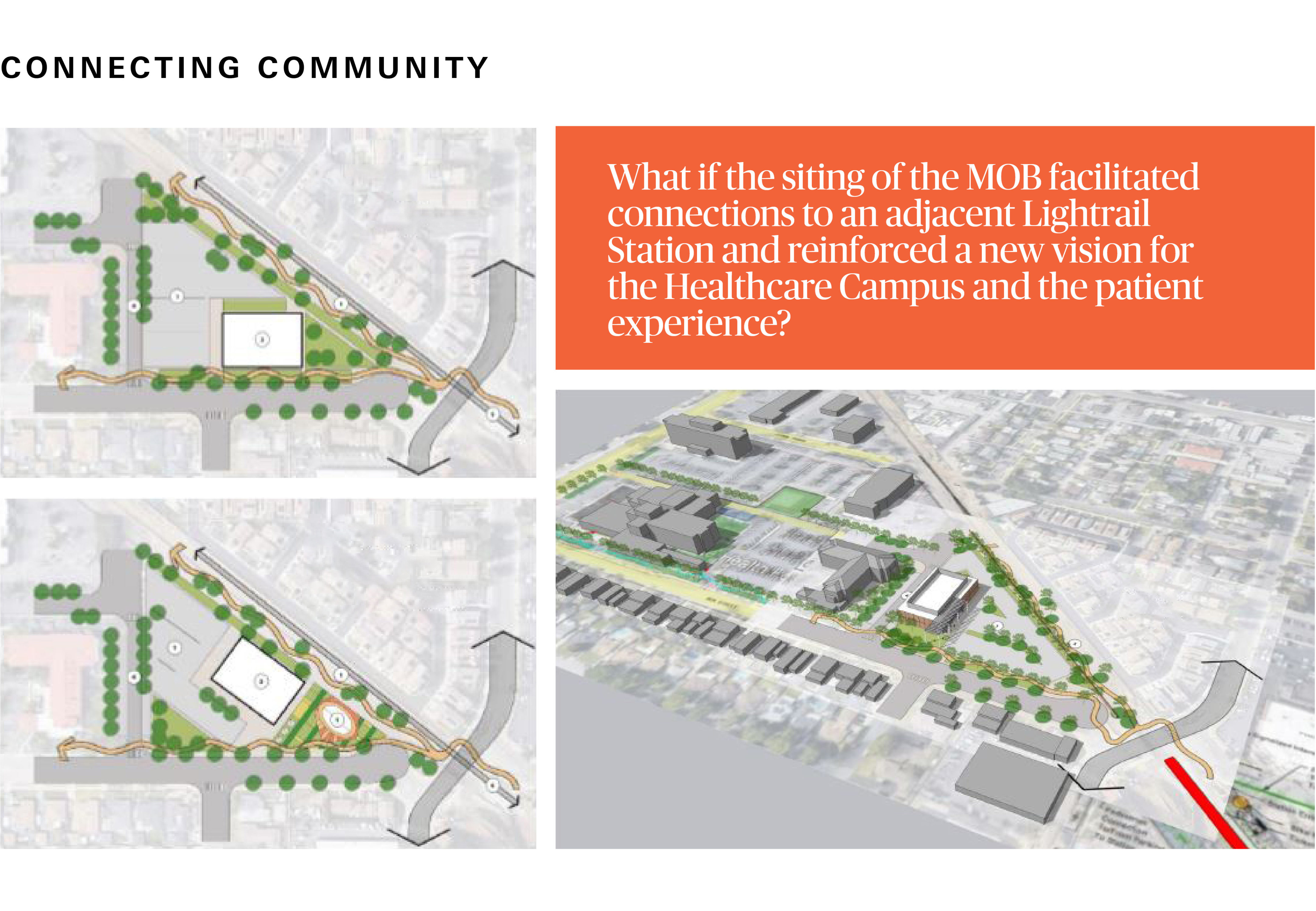
Larger providers are seeking new ways of connecting with their patients nearer to where they live. As a result, an emerging trend has been leasing or building outpatient clinics and MOB facilities in the urban core, closest to their client populations. Leasing a pre-existing office or an office building already in development is a faster way to take care directly to the community, when land value is high and vacant land is scarce. But this trend brings its own set of challenges, because often real estate is densely populated and land often already developed. MOB programs don’t easily fit into existing buildings without a significant amount of alteration and expense.
“An MOB is not a typical office building.”
“An MOB is not a typical office building,” says Keith Fine, Principal of SLAM Studio. “The infrastructure requirements are much more technical than those of a typical office building, and need to be built at a higher level of quality due to the nature of the imaging and other equipment. You have to manage your power infrastructure, cooling and vibration, among other things. It is not as challenging as a hospital building, but most MOBs have infrastructure far more complex than a typical office building.”
“The outpatient ambulatory MOB opens up the possibility of providing a large variety of services,” he continues. “When you open that spectrum up you open up the need to deal with a large variety of those issues, all are encumbered with their own specific costs.”
A hybrid approach may include leasing a space and negotiating for both interior renovations and potential additions to accommodate unique medical equipment requirements of MOBs. “We did have a client who was negotiating with a landlord about an addition on the building for an MRI,” recalls Jean Mah. “When you have larger equipment like this you can still consider leasing and attaching a specialty facility to that existing space.”
Challenges aside, locating an MOB within the community offers providers an intimate way to connect with its clients and potential client population in a way that can significantly promote better health outcomes.
Hunvey Chen, Regional Leader of Healthcare at HOK architects, worked on one such MOB where a design feature was to provide amenities that could be accessed by the community without physically entering the MOB for care. “Adjacent to the main entrance was a modular structure that we incorporated into the building that provided conference space for both the facility and the community. The area included a public coffee kiosk and a pedestrian path, landscaped and equipped with exercise equipment that anyone can use,” she says. “We were able to create something that is more available for the community – it is not just a building that you go to in order to see your doctor”
One of the challenges of leasing an existing building, or signing a lease with a developer who is building an MOB on spec is that often the investment from the provider for the buildout exceeds the investment in the lease itself – even if the lease is as long as 18 years. Given the tenant’s highly specialized build-out investment, developers know that providers rarely leave when their leases expire, hence rents tend to increase dramatically upon renewal.

Having watched this dynamic for over 20 years on the provider-side of real estate operations Bruce Rainey says that if a provider can develop its own real estate there is always a much higher ROI. Rainey is now a Vice President and the Global Solutions Leader for Jacobs Health Advisory Services. To providers seeking to create MOB facilities within communities, his suggestion is to think more like a developer than a healthcare company. “They should plan well in advance, and look for where there might be water infrastructure and transit improvements. If an organization has the insight to purchase adjacent land and hold that land – it might be off the eventual center by a few blocks, but it will give them a zone that is close enough to serve the population when density develops around those infrastructure hubs,” he explains. Going to market early and keeping some cash idling until a land opportunity presents itself promises a better ROI than waiting for communities to evolve and leasing up a building from a developer who will reap the benefit of your tenant improvement investment.
“Try to search for sites not based upon your current need. Try to project years ahead to buy land before it is desirable,” he concludes. Often, however, those opportunities are limited, and providers have to find a building within an existing community. In those cases, he suggests “try not to fall in love with a building. We often looked at multi-story buildings for office functions but they actually are very difficult to convert to MOB uses. Be particularly aware of what adjacent spaces and occupancies are. You will not be a good neighbor while retrofitting the building, and for a licensed clinic you cannot share the air with the rest of the building. You can’t do plenum air return. Most buildings developer led are plenum return, even if they are ducted. Your power requirements if you have radiology are much higher than for a basic doctor’s office as well. Data network infrastructure has to protect your PHI – so you will have to bring all of that in separately and build a separate data closet because you cannot have a shared access IT space with other tenants for patient privacy reasons.”

For the MOB whose intent is to provide outpatient surgical procedures, there are larger considerations. Fabian Kremkus, Design Principal at CO Architects explains that 25% of all surgeries can be performed as outpatient surgeries – and providers build MOBs for these because they know that it is less expensive to build and maintain outpatient operating rooms than inpatient operating rooms. However, if a patient has not recovered within 23 hours, they quickly require inpatient, not outpatient care. “A lot of times MOBs are built in close proximity to major medical centers for this reason,” he explains. But proximity may not be enough. “The communication – or even CONNECTION – between the outpatient environment and inpatient environment is super important.” This is because if an outpatient becomes an inpatient and the MOB is not physically connected to the hospital – the patient is required to be transported by ambulance – even if only across a parking lot. “I worked on an MOB project for the University of Irvine Medical Center where you wouldn’t even know if you were having a procedure in the inpatient or outpatient facility. There is a bridge that connects the two, and basically a seismic joint between them. If a patient is suffering complications and requires checking in, the care providers can simply roll her across a bridge to the hospital. The MOB is less expensive to build and the licensing of the facility is also less complicated – and they get the operational benefits for the lifetime of the facility by being the developer-owner,” he continues.
TREND 3
PATIENT & PROVIDER EXPERIENCE
Trend 3
Patient & Provider
Experience
One of the major differences between MOB and hospital functions is that an MOB has a similar throughput without the benefit of 24/7 operation. “As a designer, I’m thinking about how to treat patient traffic to make it as much of a concierge experience as possible for people arriving, coming and going,” says Fabian Kremkus. His perspective is part of a growing trend, such that many MOBs today look and feel more like hotels than they do like their hospital cousins. Scratch the surface, though, and quite a bit more attention has to be paid to throughput and back-of-house details.
“MOB design is about getting people in and out quickly,” says Fabian Kremkus. “And the MOB requires a unique attention to flow of patients and guests through the facility. Some are serving repeat visitors like oncology patients who prefer not to mix with the general public on their regular visits. They either don’t want to be seen because of how they feel or they don’t want to share space and air because they are immunocompromised. As a designer I like to treat repeat visitors as if they are VIP hotel guests.”

 “Attention to patient path of travel in and out of the MOB is critical in all cases,” he continues. “Surgical discharge areas should not be through the main entry. A separate area for discharge is nice, so that people who are recovering and feel crummy aren’t walking right out into the hustle-bustle. We sometimes separate flows by building level or building wing.”
“Attention to patient path of travel in and out of the MOB is critical in all cases,” he continues. “Surgical discharge areas should not be through the main entry. A separate area for discharge is nice, so that people who are recovering and feel crummy aren’t walking right out into the hustle-bustle. We sometimes separate flows by building level or building wing.”
“And even the path of travel for air flow is critical as it relates to the immunocompromised,” he continues. “We have to segregate the shafts – air intensive programs from non-intensive programs. Private doctor’s offices should have separate air shafts. Building a good chassis and infrastructure in the building is critical.”
Patient flow doesn’t end at the door, nor does it end at space planning. The parking and drop-off experience is equally critical to throughput, as is the signage that helps patients navigate their way from the parking lot to the front desk.
“Clear wayfinding and circulation is important,” says Mah. “Signage from the street, where the driveways are located, where the parking is relative to the entrance. All of it matters, whether the MOB is a surgery center or procedure center where people are being discharged in a more fragile condition,” she highlights.
Mah suggests considering the flow of the patient from arrival, to prep, to having the procedure, to the exit experience – preferably not through the waiting room when a patient is still recovering from a procedure. “So there’s some dignified privacy,” she continues. “The design of health facilities is just so complex, but the simpler we can make it as an end result so that people come and experience a beautiful space, the better.”
Kremkus reminds us, “you generally don’t go to an MOB because you want to be there – you go because you have to. Anything we can do to distract you or take you away from the negative aspects of why you are there is valuable. A place to take a phone call, get a little work done, get some fresh air. All of it brings humanity back to the experience.”
Finally, the experience of staff is getting a lot more attention since the unprecedented burnout years of the pandemic. “We try to design offstage and outdoor areas too for staff, both clinical and service support staff, to have respite and privacy,” says Mah. “We heard so much during COVID about the stress of healthcare, the burnout – so advocating for that staff space programmatically is so important.”
TREND 4
REAL ESTATE DEVELOPMENT VS TAKING THE CARE TO THE COMMUNITY
Trend 4
Standardization / Modularization
While the healthcare sector is an enormous behemoth – an ocean liner that is difficult and slow to steer – in many ways healthcare has boldly led trends in the broader construction industry for decades. Healthcare was really the first sector to embrace design-build and integrated project delivery models in real estate development, and LEAN practices across both medical and back of house operations. All of this to promote performance measurement and a cycle of continuous improvement.
“In the integrated, team-based care model they were implementing early on (at the Mayo Clinic) there was a holy cycle that made them get better at their practice over time – which then brought them the most complicated health cases – which made them better, and so they became the best in the world. It was LEAN for medicine,” explains Stan Chiu.
Today, influential healthcare providers are pressing forward in areas of standardization and prefabrication of construction elements to drive cost efficiencies and other organizational benefits. While there is a lot of talk about prefabrication and modular buildings in the broader construction community, healthcare companies are leaders in actually fleshing out this trend. One project leader at a major brand explains, “anything we can do to speed up the process (of completing buildings) has been part of the discussion for a decade. Implementation of tools like prefabricated systems has really taken off in the last five years or so.”
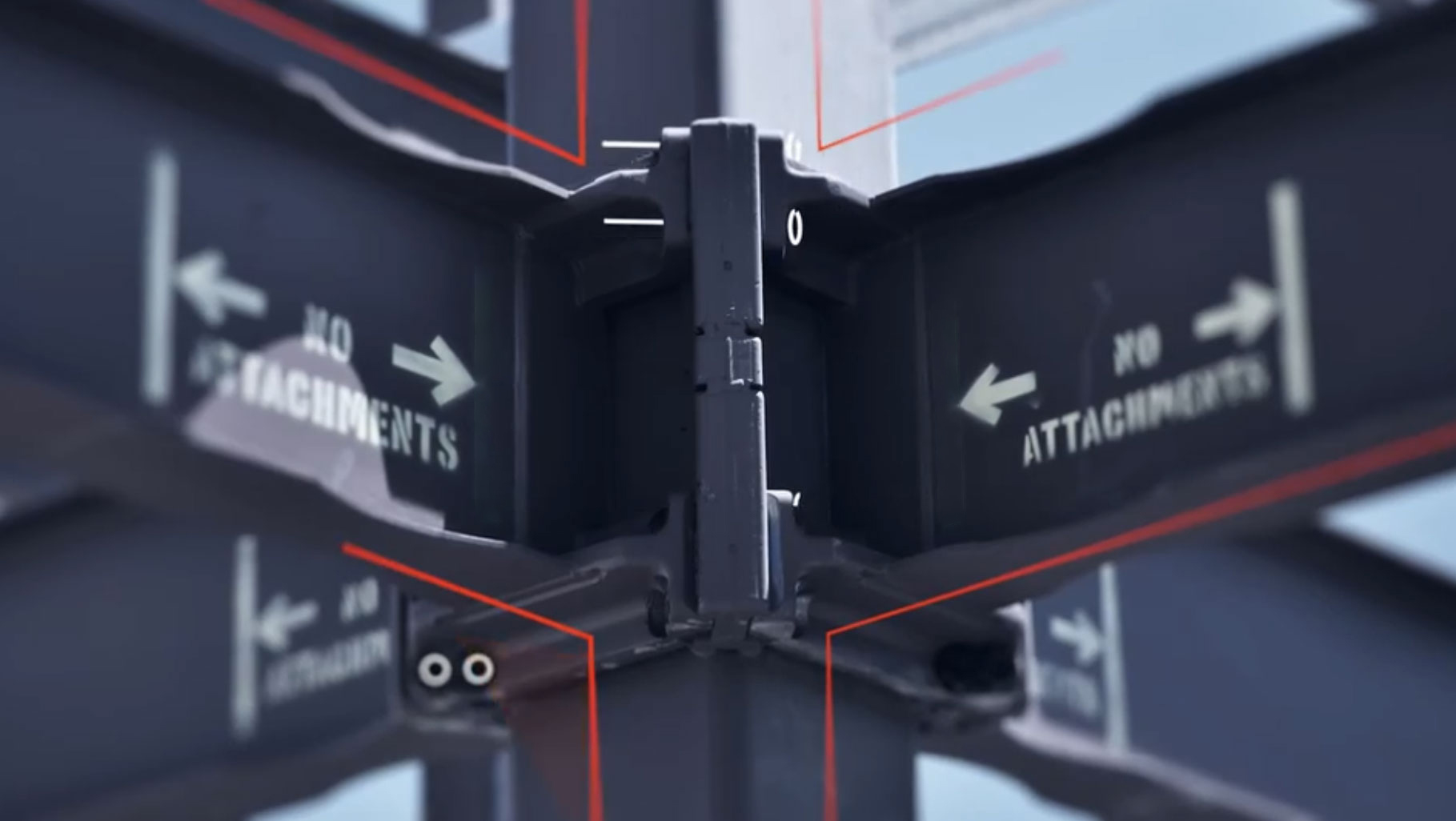
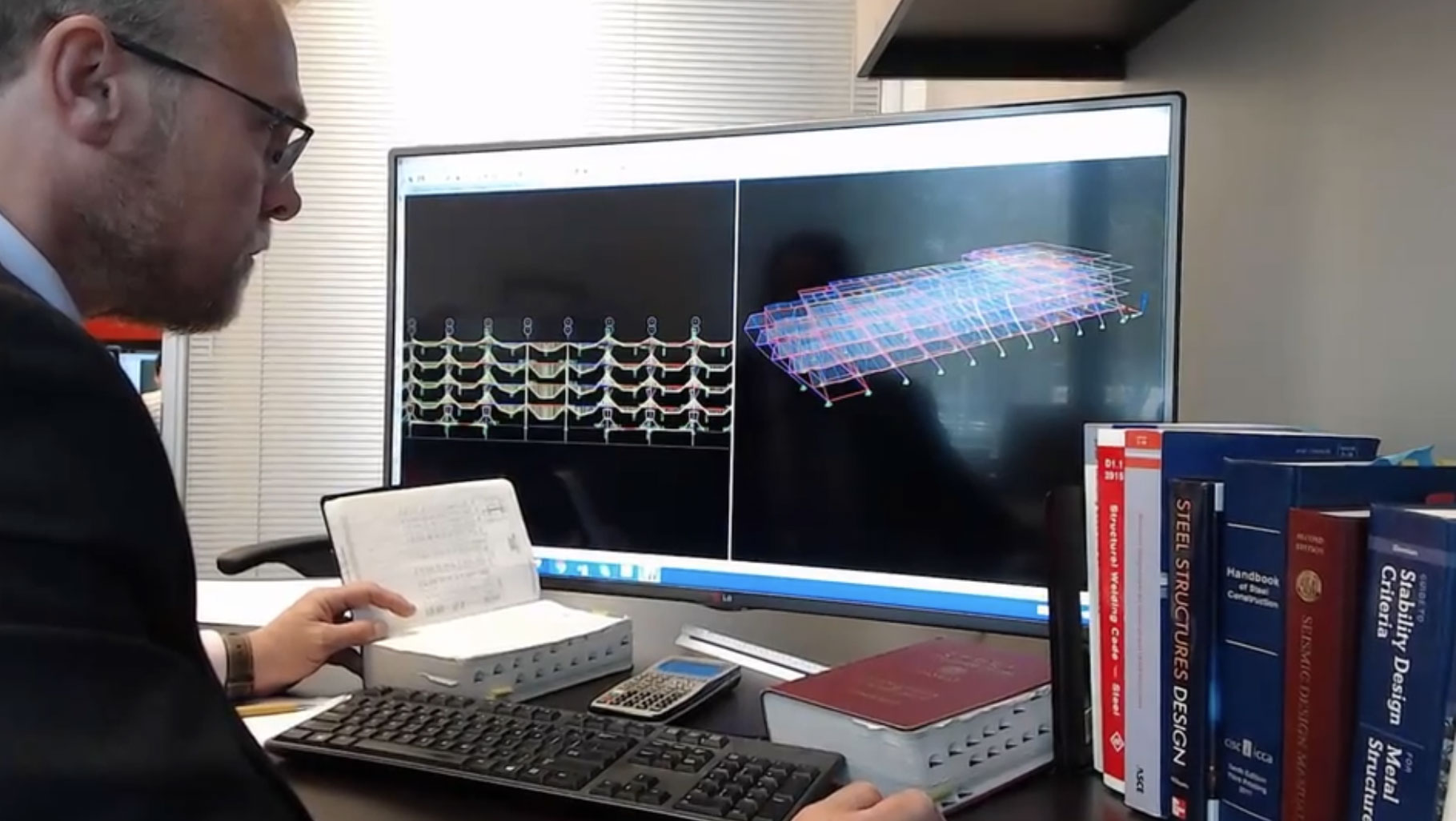
Today, several forms of prefabricated components are used for both MOB and hospital construction to accelerate building construction – and the toolkit continues to grow. Systems range from the ConXtechTM and SideplateTM prefabricated steel structural systems to fully-volumetric prefabricated bathroom pods and patient rooms. “Prefabrication as a silver bullet is a misnomer,” says Keith Fine. “There is such a spectrum of tools and approaches. “We have specified unitized curtain wall, panelized wall systems, internal demountable wall systems, prefabricated kit framing, parametric solutions – even complex assemblies like prebuilt headwalls and other patient room components. Each has its pros and cons specific to the criteria that you might have on any given project.”
Cost effectiveness of manufacturing and prefabrication is directly proportional to the scale of a project (or manufacturing order), so weighing the ROI of any given solution is critical.
“Prefabrication is extremely sophisticated and can be utilized in a wide array of spaces but doesn’t necessarily pencil out in every instance. Depending on how the system is designed and by whom, and where it’s fabricated, how it’s put together, your envelope requirement, shipping – you might find that between systems one of them works and one doesn’t. But using prefabrication you do get to take advantage of the accuracy – the tolerances are so much better than onsite construction…and (early standardization and procurement) is one way to manage the impact of cost escalation.”
“One of our largest clients is using a kit of parts for the structural systems and HVAC systems and is using standard modules and exam rooms for all of their new MOBs,” says Jean Mah. On the inside of the buildings, we are now exploring demountable partitions that can be rearranged and reused and reconfigured easily. The question is how often would the client actually do that, and so they are doing an analysis of lifecycle cost and investment in those systems. Also, what quantity of units is enough to make prefabrication cost-effective. Is 100-500 (of a module) enough? If a large healthcare provider can say this is the bathroom we’re going to use on every single project in every system it might just make sense. Then the trick is designing a bathroom – or three bathroom models that work for every building in the provider’s system,” she continues. “The occupants – the leadership, the owner of the facility, the owner of the healthcare provider and then the users themselves (the staff) – all have to agree on a single or a couple of designs.”
Beyond the potential cost and erection speed benefits of prefabricated systems, standardization of building designs is now looked at by the larger healthcare providers as a powerful way to both conserve cost and to reinforce the brand across the system, replicating the patient experience from site to site. This is particularly comforting for regular patients who need to visit MOB clinics often for treatment.
“There is a bit of a movement in Healthcare to try to develop templates and standards,” says Fine. “The more established clients have very developed standards, and others who are smaller and trying to get care more standardized and defined. They all are realizing how much it takes to develop the design from scratch on each project.”
Jean Mah adds, “…single-tenant buildings offer a nice opportunity for branding – you can have a building that is designed to suit and can allow you to carry your brand or image, or link back to your brand and building standards from your main campus. We have clients with a specific campus look at their hospitals, so when they build these ambulatory campuses they want to keep the new MOB consistent with the other campuses.”
“Most organizations are moving in the direction of standardization, and it’s a big enabler of prefabrication,” corroborates Chiu.
Modular and systems thinking from a design standpoint is also one way of future-proofing a facility, according to our advisory team.
Fine says, “a medical center is constantly being torn apart, redone and reimagined. In terms of sustainability and cost, this is not good. Lots of healthcare providers are recognizing the waste in this and are pushing their design teams hard to stop that cycle and find a solution that can switch from one modality to the next with as little waste as possible. For example, maybe the testing equipment area is isolated in a program, and the rest of the clinic can be more flexible,” explains Fine. “Maybe limit your area of modification, or use products on the interior that are more reconfigurable. If you can leave the area above the ceiling more open, with fewer obstacles it allows you to reconfigure your systems over time.”
Fabian Kremkus suggests that some prefabricated systems themselves offer flexibility by virtue of opening up the interiors. “There is a beauty to not having any brace frames (obstructing the interior). It makes the floorplans pretty flexible, and you end up with a 20’ x 20’ or 30’ x 30’ grid.”
While the industry in general is embracing prefabricated means and methods for construction, it is difficult to leverage prefabrication without early contractor study and intervention. Prefab wisdom suggests early contractor analysis is critical, as is studying schedule savings and feasibility at the earliest conceptual design milestones, to make sure that a building is designed for the systems being considered.
“Make the decision at the latest when you are at 50% SDs, but preferably in conceptual design,” says Kremkus.
Early decision-making is easier for large providers who have brought much of their own design work in-house. Chiu calls these entities “super-users,” because their organizations develop real estate at sufficient scale to drive their own changes in means and methods. “Organizations (like this) started to do the analysis themselves apart from their (outsourced) design and construction team, and then handed that work directly over to the architect and building team. The good news is that it can be faster – the bad news is that we as the outside architect are at risk for designing in a vacuum, without direct conversations with the practitioners and users of the space,” says Chiu. “There are the kinds of clients who want to do the research work themselves, and the kind who want to let us as outside teams do it for them.”
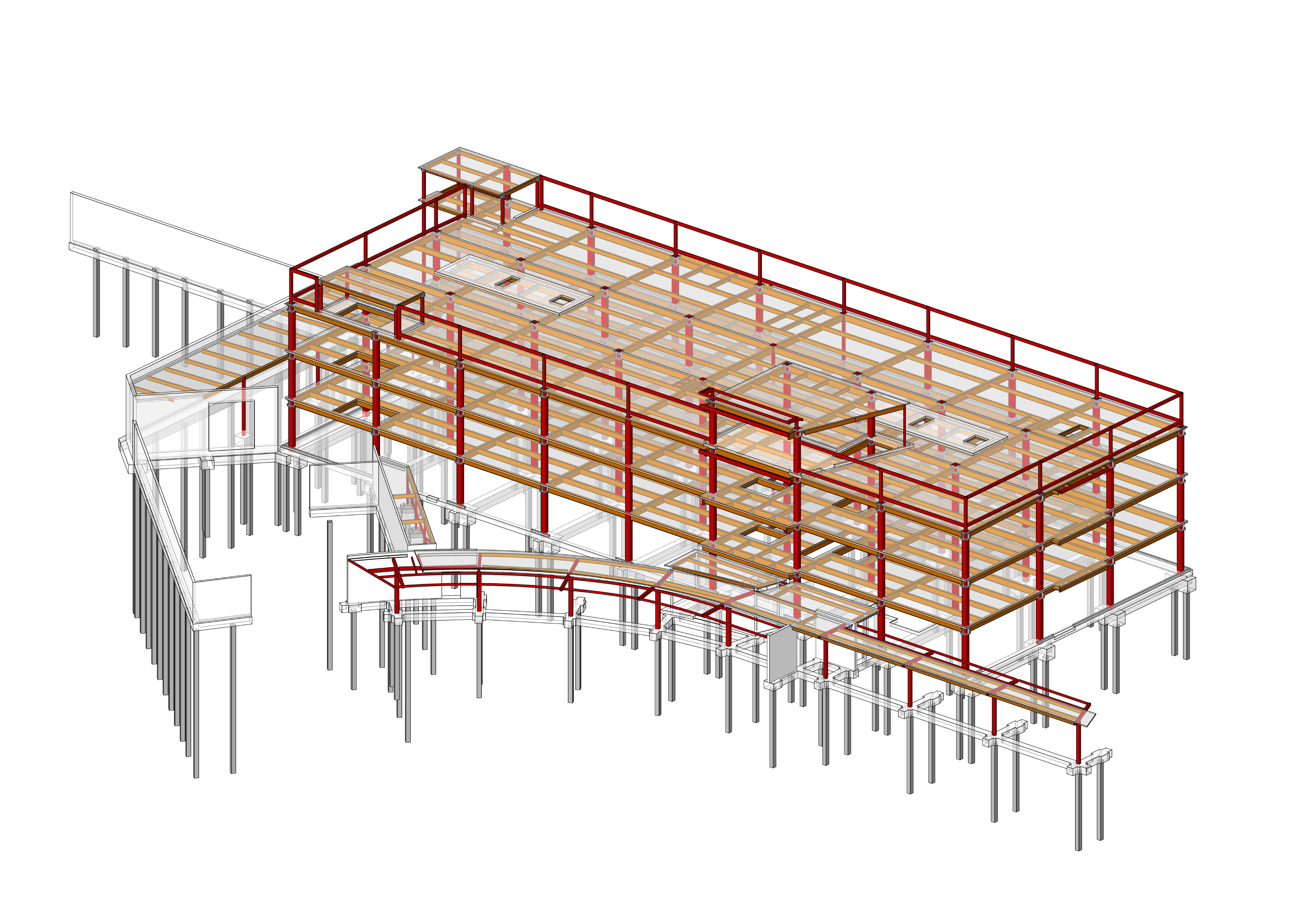
Future-proofing the MOB can be conceptualized more readily into a standardization program. “The interiors, once they are baked in, are so expensive to change in an MOB,” explains Kremkus. All of the HVAC infrastructure, any requirements for imaging, surgical rooms, etc…We found a 30’ grid is super flexible, and you can fit just about anything in it.”
CONCLUSION
Don’t do what you wanted to do yesterday.
Conclusion
MOB construction is the largest growth area in healthcare construction. Since the buildings are faster to build and less costly than hospital buildings, providers across the country are shifting as many services as possible into MOBs, from outpatient surgical procedures and imaging to low tech doctor’s consultation rooms. Along with this progressive shift to MOBs comes a rethinking of the build environment to support each facility’s specialized mission. Trends include a growing need for large flexible spaces, perimeter circulation and outdoor space. Chiu adds that this model is pushing more toward the patient, rather than primary care physician, at the center of the model. “There is a shift today toward preventative care and wellness, with the patient either a part of that team or the center of the team or even the leader of the care team,” says Chiu. “The idea is to put your healthcare money into oil changes, not engine rebuilds,” he continues. In short – the only constant is change, and with healthcare construction costs being among the highest of any building type, future-proofing is a critical part of every planning process. ”Fabian Kremkus summed it up, “Don’t do what you wanted to do yesterday. Think about what you aspire to…and hopefully 50% of that ends up in the final result.”
“Don’t do what you wanted to do yesterday. Think about what you aspire to…and hopefully 50% of that ends up in the final result.”